 Short Communication
Short Communication
Small Scale, Community Embedded Residential Aged Care – A Clinical Case Study
Rodney Jilek*
Adjunct Professor, Faculty of Health, University of Canberra, Managing Director, Community Home Australia
Rodney Jilek, Adjunct Professor, Faculty of Health, University of Canberra, Managing Director, Community Home Australia.
Received Date:November 30, 2023; Published Date:December 06, 2023
Introduction
The demographic shift toward an ageing population necessitates effective care models for older adults. Then the change in expectation from previous generations becoming more apparent as baby boomers enter care, choice and available options are becoming increasingly important considerations. Communitybased residential aged care services have emerged as a viable solution, providing tailored support within familiar environments. One of the primary advantages of community-based residential aged care is its focus on preserving and promoting independence among elders by offering highly personalized care plans tailored to individual needs, geared towards maintaining community participation and cohesion. Studies highlight that tailored assistance with daily tasks and home modifications empowers seniors to maintain autonomy in their lives [1,2]. Such programs empower older adults to maintain autonomy in their daily lives and through assistance with daily tasks, transportation services, and home modifications, elders can retain a sense of control over their routines and living environments.
Even though the number of residents in an institutional setting is significantly larger, isolation and loneliness are prevalent concerns among the elderly in these settings. Community-based care initiatives often facilitate social engagement through group activities, support networks, and access to community centers and due to their individualized, person-centered focus, loneliness can be more effectively alleviated [3]. The sense of belonging derived from these social connections contributes significantly to a better quality of life for older adults. Community-based support such as through utilizing the Community Home Model, extends beyond medical assistance and ‘care’ by emphasizing holistic well-being. It promotes healthy lifestyles through educational programs, exercise classes, and nutritional support. By addressing both physical and mental health needs, these services contribute to better health outcomes, reducing the impact of chronic conditions and hospitalizations.
A key financial advantage is that community-based care promotes community sustainability by utilizing existing community resources and fostering partnerships between various stakeholders that already exist to serve locals [4]. While community-based care alleviates the emotional and physical burden on family members in a similar way institutional residential care does, by providing respite care and support services, the additional advantage a small-scale community embedded approach has is the ability to strengthen family and social bonds and include family members and loved ones as partners in care [5, 6]. This not only benefits the elder but also helps caregivers maintain their own well-being, assists them to balance other responsibilities and provides an opportunity for continuous feedback and participation while ensuring their loved ones receive appropriate care.
A Clinical Case Study – Transition from Institutional Care back to the Community
Garry* was a resident of a mainstream 176 bed institutional residential aged care facility and had lived there for approximately nine months. During this time, his family had become increasingly concerned about his deteriorating functional status and sought alternate avenues for care. The facility was and remains fully accredited by the Aged Care Quality and Safety Commission in Australia and so it is reasonable to conclude Garry received at least the basic minimum standard of care and services that are prescribed by the current legislation and acceptable to the regulator.
At the time of his transfer to Kambera House, Garry was 67 years old. He had been diagnosed with Younger Onset Dementia and Parkinson’s Disease, both of which had been sub-optimally managed. He was unable to mobilise, required the assistance of four staff to stand up, was unable to feed himself, was doubly incontinent and was unable to speak. He had received minimal Physiotherapy and no Speech Therapy during his stay in aged care and when questioned, the staff stated he “did not have a swallowing problem” so did not require speech pathology intervention. His medications, which included the ‘do not crush’ Sinemet to control the symptoms of his Parkinsons Disease, were being crushed simply because it was deemed too difficult and time consuming for staff to get him to swallow his medication. His medical practitioner stated he had authorized this practice based upon the difficulties as expressed by the aged care staff. Garry presented in a pseudo catatonic state with a flat affect and depressed appearance and even to a layperson, looked miserable (Figure 1).
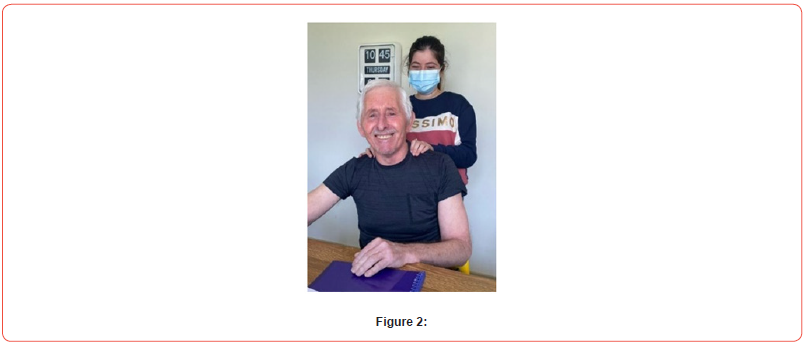
After comprehensive review by his new community based medical team, gerontological nurses, speech pathologist, dietitian, occupational therapist, pharmacist and physiotherapist, Garry was provided with an individualized program that included nutritional support, interventions to improve independence and function, a new medication regime and daily exercises to improve mobility. This program was delivered by our specially trained dementia care companions coordinated by a Registered Nurse, all completed in the community and without acute care hospital intervention. Five weeks after the commencement of this program, Garry was able to stand with the assistance of one team member and had begun mobilizing with the use of a walking frame. His speech was returning, and his effect improved dramatically. With assistance to complete toileting tasks, his level of continence improved. It is noted that this was all undertaken during the COVID pandemic (Figures 2 & 3).
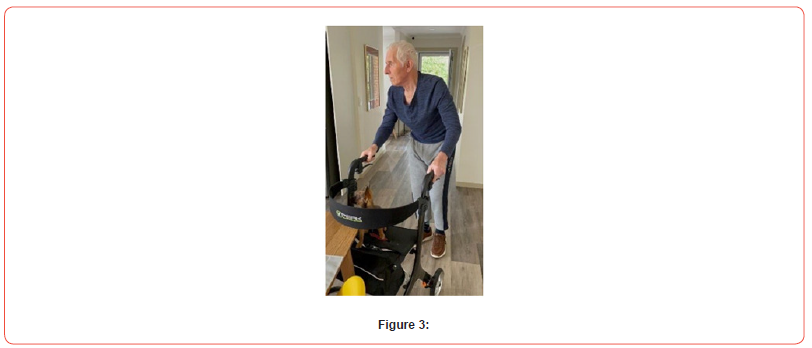
The program of support, underpinned by the Community Home Model, encouraged a relationship approach that enabled the guest, their loved ones and the support team to build a meaningful connection that surpasses the delivery of clinical care. The team was empowered and encouraged to love, show love and share in the beauty of their guests’ lives. Family becomes an integral part of the support program and work together with our team to develop and implement highly individualized programs of support. Over the next 12 months, Garry continued to improve and was able to mobilize throughout the house independently using his frame and also outside with only supervision and monitoring. He resumed his community-based life, participating in community events and engaging socially with others at Club Kalina, a community embedded day program for people living with younger onset dementia and cognitive disability.
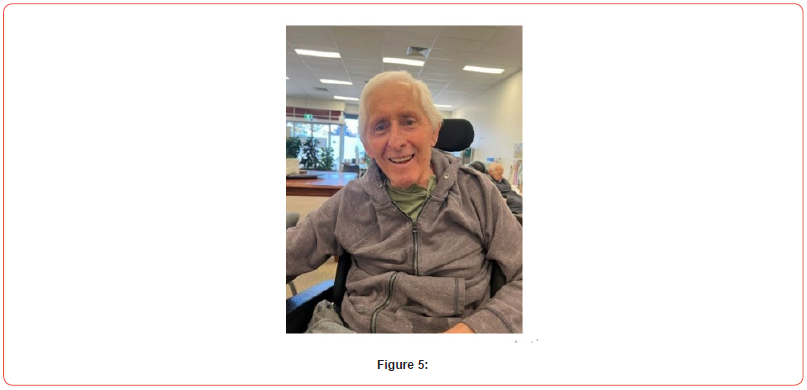
Even as his health continued to decline, Garry enjoyed a range of pursuits and activities and remained an active participant in life (Figures 4 & 5). Garry passed away in Kambera House, surrounded by his family and loved ones in November 2023 having spent his final two years living in his local community. His end-of-life care, which included the use of multiple syringe drivers and intensive clinical support was delivered in consultation with the specialist palliative care team at Clare Holland House by our Registered Nurses and her amazing companion team at Kambera House. His family were an ever-present part of his life and actively involved in every step of his journey.

Conclusion
Through Garry’s powerful story we can easily identify the many advantages of person-centered care delivered in a small scale, community-embedded setting. The ability to remain connected to one’s community and receive support that is flexible, timely and individually tailored to a singular persons care needs ensures the best possible clinical and psychosocial outcomes for the guest and enables them to live their best life.
Acknowledgement
“The family of Mr Garry Brown who have kindly consented to the publication of Garry”s story”.
Conflicts of Interest
No conflict of interest.
References
- Laura N Gitlin, Laraine Winter, Janice Burke, Nancy Chernett, Marie P Dennis, et al. (2008) Tailored Activities to Manage Neuropsychiatric Symptoms in Persons with Dementia and Reduce Caregiver Burden: A Randomized Pilot Study. April 2008 American Journal of Geriatric Psychiatry 16(3): 229-239.
- Greenfield EA, Scharlach A, Lehning AJ, Davitt JK (2012) A conceptual framework for examining the promise of the NORC program and Village models to promote aging in place. J Aging Stud 26(3): 273-284.
- Victor C, Scambler S, Bond J, Bowling A (2000) Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol 10(4): 407-417.
- Szanton SL, Thorpe RJ, Boyd C, Tanner EK, Leff B, et al. (2011) Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health- related quality of life in disabled older adults. J Am Geriatr Soc 59(12): 2314-2320.
- KE Pani-Harreman, Joop MA van Duren, Gertrudis IJM Kempen, Gerrie JJW Bours (2022) The conceptualisation of vital communities related to ageing in place: a scoping review. European Journal of Ageing 19(1): 49-62.
- Fields B, Yanes C, Ennis M, Toto P (2022) Community Aging in Place, Advancing Better Living for Elders (CAPABLE) program: Understanding the potential involvement of care partners. Health Soc Care Community 30(4): e1212-e1219.
-
Richard M Monaghan*. Metabolism And Proteostasis: At the Intersection of Inflammation- Associated Decline in Health span. Glob J Aging Geriatr Res. 2(4): 2023. GJAGR.MS.ID.000546.
-
Comorbidity; Elderly; Prevalence.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






